Prostatitis is an inflammation of the prostate gland (prostate) and is an extremely common disease. According to various sources, 35-45% of the stronger sex encounter it. Moreover, the disease predominantly affects men aged 20 to 50 years, that is, in the prime of life, during the period of active sexual life.
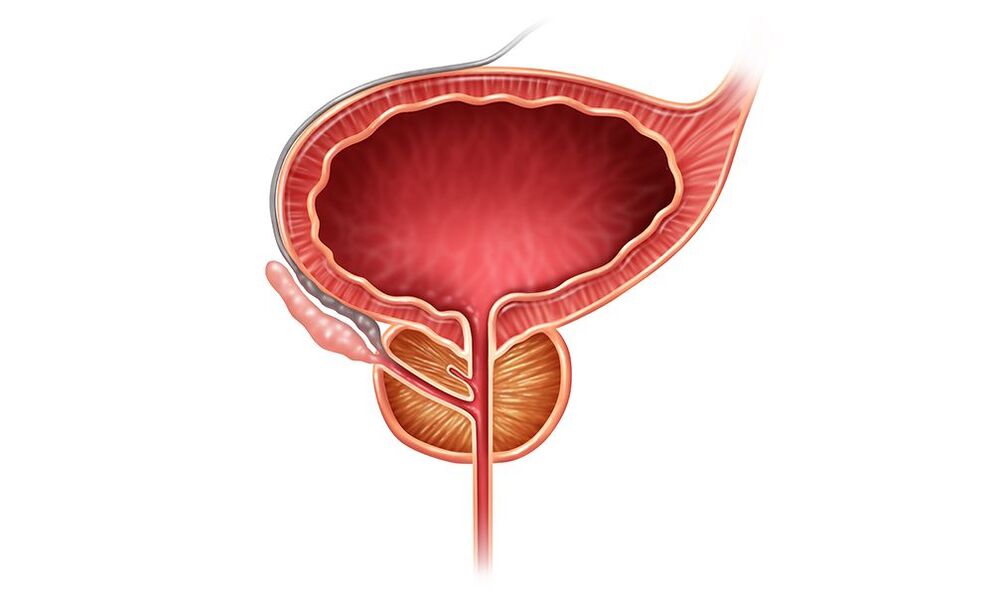
The main function of the prostate is to participate in the formation of sperm. Its numerous glandular lobules secrete a secretion that makes the sperm fluid, less viscous, and provides nutrients to the sperm, ensuring their activity and vitality. The seminal fluid flows into the prostate, is enriched with this secretion, and during arousal is poured into the urethra (urethra). The muscle fibers of the prostate are involved in "pushing out" sperm during sexual intercourse. Thus, prostate diseases, incl. prostatitis, affect the male genital area, affect potency, worsen the quality of sperm, and reduce the ability to fertilize.
The prostate is located in a tight space limited by the pelvic bones, next to other organs that are involved in the daily functions of a person. Therefore, inflammation of the prostate affects other physiological processes. Thus, the upper part of the urethra (urethra) passes through the prostate gland, so prostate disease often leads to problems with urination in men, which become frequent, and the process itself is painful and difficult. The back of the prostate is closely adjacent to the wall of the rectum, so when it is inflamed, constipation may also occur.
Prostatitis has symptoms similar to other genitourinary diseases (prostate adenoma, cystitis, urethritis, etc. ), therefore, for proper treatment if you experience discomfort in this area, you must immediately consult a urologist.
Types of prostatitis
According to the severity of the inflammatory process and the duration of the disease, prostatitis is divided into two types: acute (the duration of which is no more than 3 months) and chronic. The causes of acute prostatitis, features of changes in the gland at different stages, symptoms are well studied, and quite effective treatment methods have been developed. Regarding chronic prostatitis, today there are more questions than answers - this applies to both diagnosis and treatment of the disease.
Acute prostatitis: symptoms, stages, causes
Acute prostatitis occurs in 5-10% of men, most often aged 20-42 years. With proper treatment, the disease lasts no more than 3 months. The symptoms of prostatitis are very pronounced, which in most cases forces the patient to immediately consult a doctor.
Acute prostatitis is characterized by the following striking symptoms:

- Local manifestations are pain in the lower abdomen, perineum, glans penis, rectum, pain can radiate to the lower back and tailbone. Due to inflammatory swelling of the prostate, the lumen of the urethra passing through the gland narrows, causing difficulty and pain when urinating. Acute urinary retention may develop, in which the patient cannot urinate on his own (hospitalization and catheter insertion are required).
- General – high temperature, weakness, thirst, nausea, vomiting, clouding of consciousness, etc.
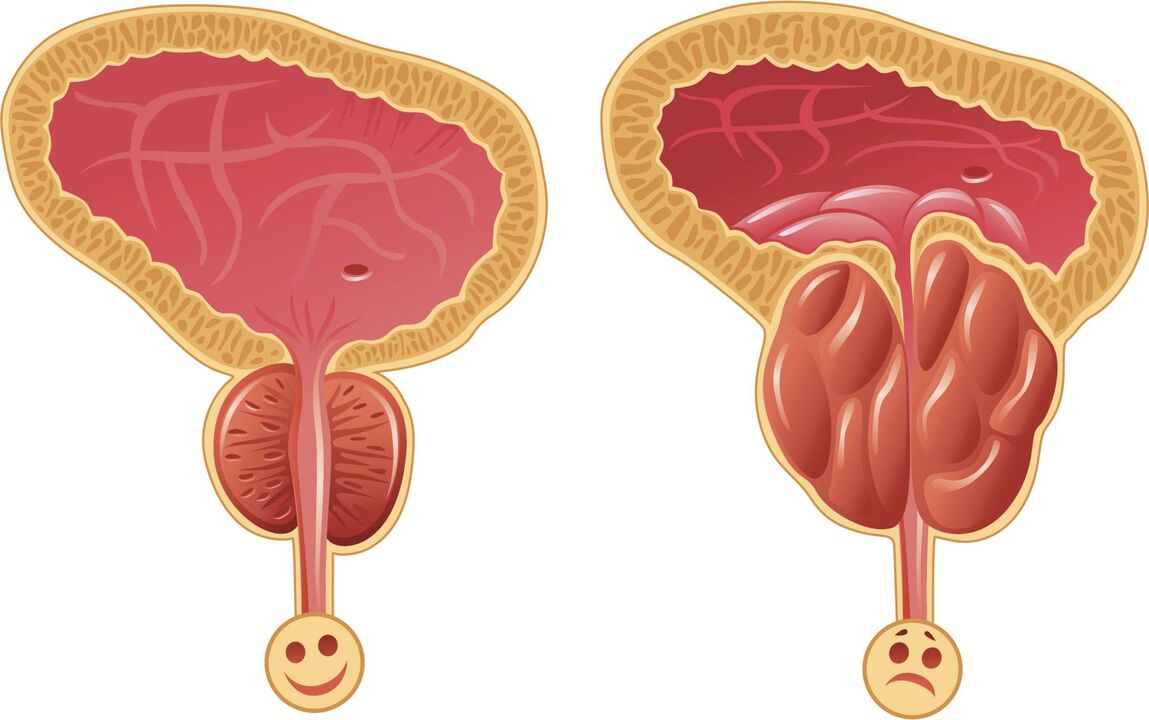
There are three forms (or otherwise they can be called stages) of acute prostatitis: catarrhal, follicular and parenchymal. An abscess (ulcer) of the prostate gland is also identified as a separate form (N. A. Lopatkin, 2002). They differ in the depth of damage to prostate tissue, the severity of the inflammatory process and symptoms of the disease:
- First, the mucous membrane of the excretory ducts is affected - the tubules through which prostate secretions are discharged into the urethra. Catarrhal prostatitis develops.
- The glands themselves, which are responsible for the production of secretions, are involved in inflammation - follicular prostatitis.
- Inflammation spreads to most of the organ - parenchymal prostatitis develops.
- The course of acute prostatitis can be complicated by the development of an abscess - a prostate abscess. This is the most dangerous form of the disease, because. . . in the absence of proper treatment, the infection can enter the bloodstream - microbes spread throughout the body and infect the blood (sepsis develops) with a high probability of death.
Causes of prostatitis
The main cause of acute prostatitis is infection. In most cases, pathogens enter the prostate from the urethra along the ascending tract. These could be:
- sexually transmitted infections: gonococci (causative agents of gonorrhea), chlamydia, trichomonas, ureaplasma, etc. They are the most common causes of acute prostatitis in young men 20-30 years old who are promiscuous;
- opportunistic microorganisms, that is, microbes that can be constantly present in the body, but become active only when general and local immunity decreases. The most common are Escherichia coli, and the "culprits" can also be Klebsiella, Proteus, and, less commonly, streptococci, staphylococci, etc. More often, this cause is diagnosed in men over 40 years of age.
Much less frequently, microbes (for example, staphylococci) can enter the prostate in other ways:
- with the flow of blood or lymph from purulent foci in the body (chronic tonsillitis, sinusitis, boils, carious teeth, etc. ). In this case, acute prostatitis can begin immediately with an abscess (ulcer);
- from the urethra along the descending tract, when there is inflammation of the bladder (cystitis), kidneys, and upper urinary tract;
- during various therapeutic and diagnostic manipulations in the prostate gland (insertion of a catheter into the urethra, administration of medications, etc. ). Through injured areas, the infection enters the prostate.
However, infection is not the only cause of inflammation. The prostate gland is an organ well protected from microbial invasion; its sterility is maintained thanks to the work of the general immune system, as well as local defense mechanisms: prostate secretion has the ability to destroy microbes that have entered the organ. Therefore, for the development of infection in the organ, certain conditions must be created.
A favorable environment for the development of microbes is the accumulation of dead cells in tissues, which, due to their protein content, are an excellent breeding ground for infection. For example, the infection can feed on stagnant prostate secretions remaining in the excretory ducts as a result of incomplete ejaculation. In this regard, for effective treatment of prostatitis and its prevention, it is necessary to pay attention to congestive processes in the pelvis and the causes of their occurrence.
Chronic prostatitis: symptoms, causes
Chronic prostatitis has a long-term (more than 3 months) recurrent (recurring) nature. The disease has a number of unpleasant symptoms:
- Urinary dysfunction. Due to inflammation, the nerve endings in the urethra are irritated, which leads to a frequent urge to urinate (especially at night), a sudden and imperative urge, and urinary incontinence. At the same time, the process of urination itself is difficult and may be accompanied by cutting pain, since the urethra is compressed due to swelling of the gland.
- Sexual function disorders. During sexual intercourse, there is faster ejaculation and pain during or after this process. Erection weakens and libido decreases. Long-term illiterate treatment can lead to impotence and infertility.
- Pain that the patient experiences not only in the genitals and pelvis (testicles, glans penis, perineum, rectum), but also in the lower back, on the inside of the thighs.
- Prostatorrhea, when prostate secretion is released from the urethra outside of sexual intercourse. This is due to a weakening of the muscle tone of the excretory ducts of the prostate, due to which the secretion flows freely into the urethra. With bacterial prostatitis, the secretion may be mixed with pus, and with calculous prostatitis (with the formation of stones) – with blood.
- Depressive states, increased fatigue, anxiety, etc. Some are so emotionally absorbed by the disease that they are no longer interested in anything, which leads to the loss of their job, the destruction of their family - "going into illness with a separation from reality. "
Stagnant processes in the pelvis
So, the main prerequisite for the development of prostatitis (both acute and chronic) is congestion in the pelvis. Only in very rare cases can autoimmune or hormonal disorders be the root cause of prostatitis.
Congestion may be local in nature and relate only to stagnation of prostate secretions. It can form due to frequent practice of interrupted coitus, masturbation, or due to prolonged abstinence, because regular sex life and full sexual intercourse are very important for a man’s health. With masturbation, incomplete ejaculation occurs due to a sitting, stationary position, since the force of ejection of seminal fluid depends on good blood circulation to the area, which must be ensured by the active work of the pelvic muscles.
The secretion remaining in the excretory ducts thickens and clogs them, thereby preventing the release of new secretions. In this case, the stagnant secretion loses its bactericidal properties, i. e. ability to destroy microbes. The cells contained in the secretion die and their decay particles (protein) become a breeding ground for infection. This is especially important to understand in cases where prostatitis is caused by opportunistic flora (for example, E. coli), which is often present in the body, but is activated only under favorable conditions - with the accumulation of dead cells.
However, stagnation of secretions due to less than ideal sex life is not the only cause of prostatitis, especially if we are talking about chronic prostatitis or old age. A significant role is played by stagnation of blood and lymph in the pelvis, which also leads to the accumulation of dead cells and other negative changes in tissues.
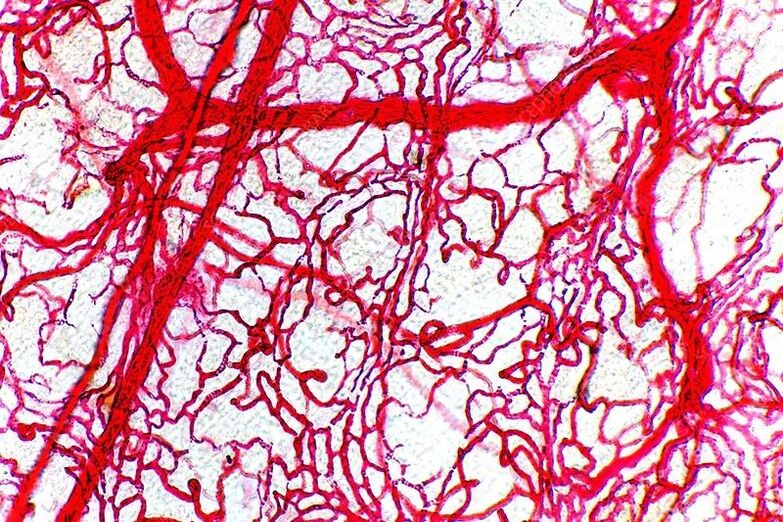
As you know, all tissues of our body consist of cells. The cells of the body are constantly dying and being damaged (under the influence of toxins, shock loads, hypothermia, edema, etc. ). However, with sufficient lymph flow (movement of lymph through the vessels of the lymphatic system), dead cells are removed from the tissues, freeing up space for the growth of new functional cells, that is, cells that perform the main function of the tissue (for example, for the prostate glands - secretion production, for muscle cells -ability to contract).Due to venous stagnation, swelling of the pelvic organs, including the prostate, occurs. In a tight space limited by the pelvic bones, such an overflow of blood leads to pinching of blood vessels (correspondingly, nutrition deteriorates), compression of the prostate excretory ducts, etc. Cell death accelerates.
The main reason for stagnation is physical inactivity (sedentary lifestyle). It is not without reason that the disease is more common among those who spend a lot of time driving a car, among office workers, and among those who, due to health problems, cannot lead an active lifestyle. Today, there is a deeper understanding of why a sedentary lifestyle has such a detrimental effect on human health, contributing to the development of not only prostatitis, but also constipation, prostate adenoma, cystitis, etc.

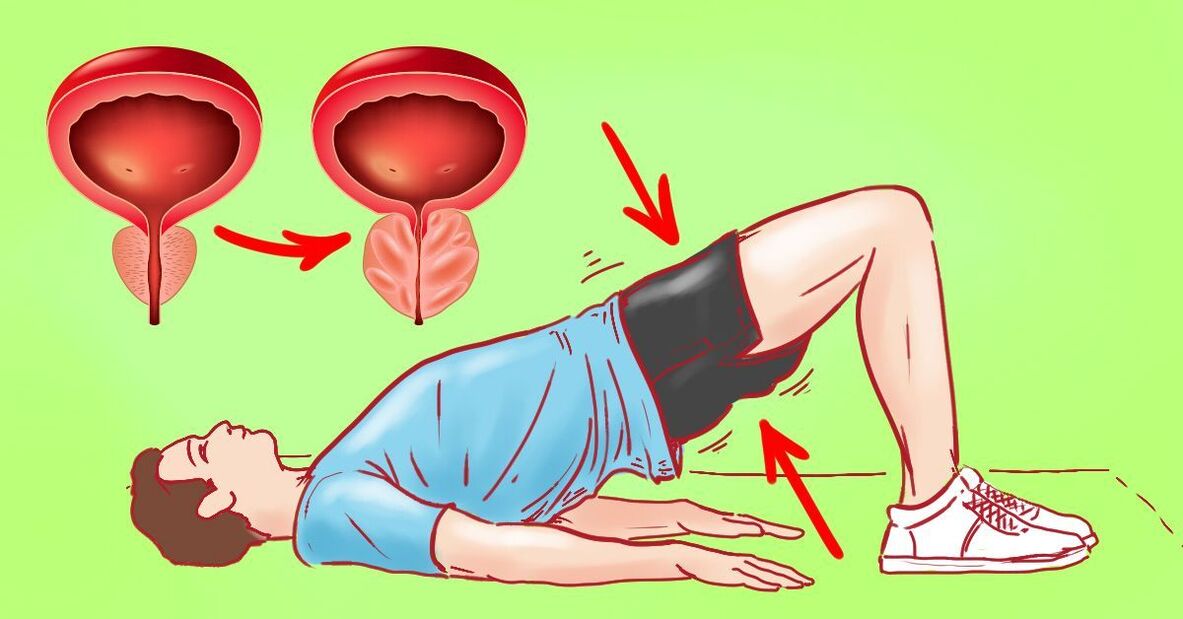
During physical activity, skeletal muscles tense and create biological microvibration energy* due to the alternating contraction of muscle fibers.
Biological microvibration is a vital condition for many transport and metabolic processes in the body, in particular for (a) lymph flow and (b) venous outflow, as well as for the normal functioning of the kidneys and liver (c).
(a) Unlike the circulatory system, the lymphatic system does not have a pump (heart), and most vessels do not have a muscular "wall" to compress the vessels and push the lymph forward. The movement of lymph is ensured by the work of muscle tissue located next to the vessels (skeletal muscles or the muscular "shell" of other organs). In the area of the prostate gland, lymph flow is ensured by microvibration of the pelvic floor muscles, bladder and peristalsis (wave-like contraction) of the rectum. That is why "inactivity" of the pelvic muscles and constipation (which indicates weak peristalsis) lead to stagnation, accumulation of dead cells, and, as a result, to prostatitis.
(b) Most venous vessels have their own muscular walls. However, their contractile activity is similarly "encouraged" by the work of skeletal muscles, because the pushing power must be sufficient for the venous blood to overcome gravity, returning to the heart. Otherwise, the tone of the muscle walls of the venous bed decreases, and in the presence of additional damaging factors, venous disorders develop, including the formation of venous stagnation.
(c) Due to a sedentary lifestyle, the function of the kidneys, which are responsible for the water and electrolyte balance of the blood, suffers. This blood parameter directly affects the contractile activity of all muscle tissues of our body (skeletal muscle tone, tone of the bladder, intestines, prostate excretory ducts, etc. ). Kidney performance depends on the dynamic work of the back muscles and general physical activity. Similarly, the quality of blood purification from toxins and other waste substances depends on the performance of the liver.
Muscle tissue creates microvibration energy constantly and regardless of our physical stress, even at rest (when we sleep). However, it is during physical activity that the necessary power and frequency of microvibration develops.
Conclusion: Regular sex life and physical activity are necessary conditions for the prevention and treatment of prostatitis, since it is during physical muscle tension that biological microvibration energy arises, which prevents stagnation of secretions, venous blood and lymph in the pelvic organs.
Drug therapy

Drug therapy is most effective in the treatment of acute prostatitis and usually includes:
- Antibiotics and other medications to fight infection. Since tests to determine the type of microbes that caused acute inflammation take more than a week, and the patient’s acute condition does not allow for a long wait, treatment is often started "blindly. "Initially, broad-spectrum antibiotics are prescribed, and based on the results of bacteriological testing, treatment can be adjusted.
- Antipyretics and painkillers to alleviate the patient's condition.
- Alpha blockers and similar drugs. They reduce muscle tone, forcibly relieve swelling in the prostate gland, and thereby facilitate the process of urination.
- Taking large amounts of fluids (saline) to cleanse the body of toxins that poison the entire body.
The antibiotic purposefully destroys the infection, the proliferation of which causes an acute reaction in the body, and the patient’s condition improves. However, in the absence of sufficient lymph flow, tissue cleansing from dead cells and toxins does not occur in the pelvic organs, and therefore there remains a risk of subsequently developing chronic prostatitis.
Drug therapy for chronic prostatitis includes:
- Also antibiotics and other medications, despite the fact that in most cases the infection is not detected. There is always a risk that the tests simply did not diagnose the infection, so it is necessary to take measures that will prevent the spread of this undetected infection. According to studies, up to 40% of patients with chronic prostatitis who did not have a bacterial infection have improved as a result of using antibiotics.
- Nonsteroidal anti-inflammatory drugs that "block" the body’s inflammatory response. Long-term use of them negatively affects the mucous membrane of the gastrointestinal tract and the entire body in general.
- Alpha blockers to improve urination. The effect of treatment is achieved with long-term use (at least 6-8 months).
Prostate massage
Massage of the prostate gland is carried out from the inside - through the rectum using a finger. There are cases when people try to perform massage at home on their own (sympathetic relatives). However, an effective massage is not just massaging this area, but influencing different parts of the prostate in strict sequence and in a certain direction. In this regard, competent and effective massage can only be performed by a urologist.
Prevention of prostatitis
Twenty years ago, prostatitis was considered a disease of middle age, as it was rarely diagnosed in men under forty years of age. Today, acute inflammation of the prostate gland is not uncommon among twenty-year-olds. And chronic prostatitis is observed in 45% of men aged 25 to 50 years.
Prostatitis is accompanied by painful symptoms (fever, pain, difficulty urinating, erectile dysfunction), leads to complications such as cystitis, pyelonephritis, infertility and, of course, seriously affects the quality of life.
Therefore, today men are increasingly interested in ways to prevent prostatitis.
Who needs prostatitis prevention?
There are groups of men whose risk of developing prostatitis is higher than others.
- Men over 45 years old.
- Representatives of sedentary professions: programmers, IT specialists, office workers, accountants, economists, etc.
- Drivers, lovers of long bicycle trips, and also often using air transport.
- Men who are temporarily or permanently exposed to unfavorable weather conditions: low air temperature and high humidity. For example, those working on a rotational basis in the northern regions, climbers, high-rise builders, ski fans, etc.
- Suffering from chronic infectious diseases.
- Smokers.
However, given the fact that the disease is rapidly getting younger, all men should take measures to avoid encountering prostatitis in the future.
Prevention of prostate inflammation includes many recommendations. A man can follow all of them or some of them. Experts believe that even partial compliance with the recommendations reduces the risk of this disease.
Diet for the prevention of prostatitis
All doctors talk about the role of nutrition. Unfortunately, very often the recommendations are general. But in the case of prostatitis prevention, diet really plays an important role. The fact is that a diet to prevent problems with the prostate gland should solve several specific problems, and not just "strengthen the body. "
Proper nutrition to protect against prostatitis has the following goals:
- Reduce prostate irritation that occurs after eating certain foods.
- Improve blood circulation in small and large capillaries.
- Normalize digestion to eliminate constipation and other gastrointestinal disorders. Constipation is one of the factors in the development of prostatitis.
- Provide a favorable environment for the development of natural intestinal microflora.
What foods harm the prostate gland and increase the risk of prostatitis?
- All types of peppers and sauces with them, horseradish, onions and other hot seasonings: they irritate the prostate tissue and cause inflammation.
- Citrus fruits, especially lemons and grapefruits, sour fruits and berries have a bad effect on the condition of the prostate and reduce its resistance to infections.
- Strong alcohol causes a narrowing of the already narrow ducts of the prostate, causing stagnation of secretions, a direct consequence of which is prostatitis.
- Carbonated drinks and fermented drinks with gases (kvass, beer) also irritate the prostate gland.
- Dishes from legumes (pea soup, beans, etc. ), mushrooms and offal: are difficult to digest, slow down intestinal motility and cause gas formation and constipation.
- Bacon, lard, and fried foods increase the level of cholesterol in the blood, which impairs blood circulation, including in the pelvic organs. It is this phenomenon that often becomes the leading cause of the development of prostatitis in men.
What foods are useful for preventing prostatitis?
- Seafood and fish at least once a week. They contain important amino acids and omega polyunsaturated fatty acids, which are necessary for the normal functioning of the prostate gland and its ability to resist inflammation.
- Parsley and parsnips (greens and roots) can be added to food as a seasoning in dishes, especially in the summer. The positive anti-inflammatory effect of these spicy plants on the prostate has been proven by numerous studies.
- Cabbage of all types (cabbage, kohlrabi, collards, cauliflower, Brussels sprouts), radishes, turnips – several times a week if possible. Studies have shown that when consumed regularly, these vegetables prolong men's health and protect against age-related changes in the prostate gland.
- Low-fat fermented milk products - at least 2-3 times a week. They are needed to normalize intestinal motility and maintain beneficial microflora.
- Antioxidants, especially rutin, vitamins C and E, beta-carotene and lutein - a thirty-day course once a year or more often. Antioxidants protect prostate tissue from the effects of inflammation, increase the prostate's ability to resist infections, and also improve blood circulation in small capillaries and slow down age-related disorders in tissues.
Important! As for recommendations to eat nuts, pumpkin seeds or bananas, since they are rich in essential vitamins and antioxidants, experts are of the same opinion: the products do not contain enough of these micronutrients to provide the body with them.
If a man loves nuts or seeds, then he can safely include them in his diet; these products will not cause harm, but they will not significantly affect the condition of the prostate gland. When it comes to preventing prostatitis, it is much more effective to use complexes high in antioxidants and vitamins.
Lifestyle – what to pay attention to?
If a man smokes, giving up this habit will significantly reduce the likelihood of developing prostatitis. Smoking seriously impairs venous outflow, which leads to tissue swelling, stagnation of blood and lymph. General blood circulation in the pelvic organs slows down, the prostate gland receives insufficient nutrition and oxygen, and its normal functioning becomes impossible.
Regular sex life plays an important role in the prevention of prostatitis. This is the main way to prevent congestion in the prostate gland. However, it is important to use condoms when having sex.
With a sedentary lifestyle, a man should introduce more physical activity into his life. Swimming, tennis or running are suitable, as are regular walking or avoiding using the elevator.





































